An Easy Guide to Isolation & Surgical Gowns [FAQs]
Gowns are the second-most-used piece of PPE in healthcare settings, following disposable gloves.
But when COVID-19 happened, global supply chains were hit hard. Healthcare facilities found themselves with a shortage of PPE — including gloves and isolation gowns.
Manufacturers scrambled to meet the increased demand. But with so many products out there, it was harder for healthcare institutions to discern which ones would adequately protect their workers.
How do you know what type of isolation gown you need — or whether the product you’re looking at is up to the task?
We’ll answer these questions and more in this guide.
1. What Are Isolation Gowns?
Isolation gowns are Personal Protective Equipment (PPE) that cover the torso, arms, and clothing. They act as a liquid barrier against blood, bodily fluids, and other infectious materials.
The gowns serve two purposes: to protect healthcare workers from potential contaminants and to prevent healthcare workers from transferring microorganisms that could harm vulnerable patients.
Isolation gowns are worn during procedures and patient-care activities where the healthcare worker anticipates contact with patient clothing, blood, bodily fluids, secretions, and excretions. The type of isolation gown necessary depends on the nature of the patient interaction and the level of risk present. (More on this below)
You’ll sometimes find isolation gowns referred to as “protective gowns,” “precaution gowns,” and “cover gowns.” But the FDA does not recognise these terms in their classification of medical devices, and many of these do not adequately protect wearers.
For example, cover gowns sometimes refer to isolation gowns with no barrier, but both the AAMI and FDA definitions of isolation gowns are PPE meant to protect healthcare professionals and patients from the transfer of microorganisms and bodily fluids — in other words, they have a barrier.
To be sure that your isolation gown will properly protect you, check that the AAMI standards and levels of protection are appropriate for the task.
2. What Types of Isolation Gowns Are Available?
According to the FDA, there are two main types of isolation gowns:
- Surgical isolation gowns
- Non-surgical isolation gowns
However, there are also clean and sterile versions of these along with differing levels of barrier protection.
Surgical Isolation Gowns
Surgical isolation gowns provide protection in medium to high-risk situations, such as during arterial blood draws, insertion of IV lines, fluid-intense procedures, or the suspected presence of non-airborne infectious diseases.
Compared to surgical gowns, surgical isolation gowns have larger critical zones. This means that aside from the bindings, cuffs, and hems, every part of the gown must provide the highest level of liquid protection for which the gown is rated.
Surgical isolation gowns are regulated as a Class II medical device and require FDA approval before they can be marketed as such.
Non-surgical Isolation Gowns
Non-surgical isolation gowns have the same critical zones as surgical isolation gowns. The difference is that non-surgical gowns are Class I medical devices and therefore do not need FDA approval.
Non-surgical isolation gowns are only worn when there’s little to no risk, such as during basic care, standard isolation, as a cover gown for visitors, or in a standard medical unit.
3. What Types of Surgical Gowns Are Available?
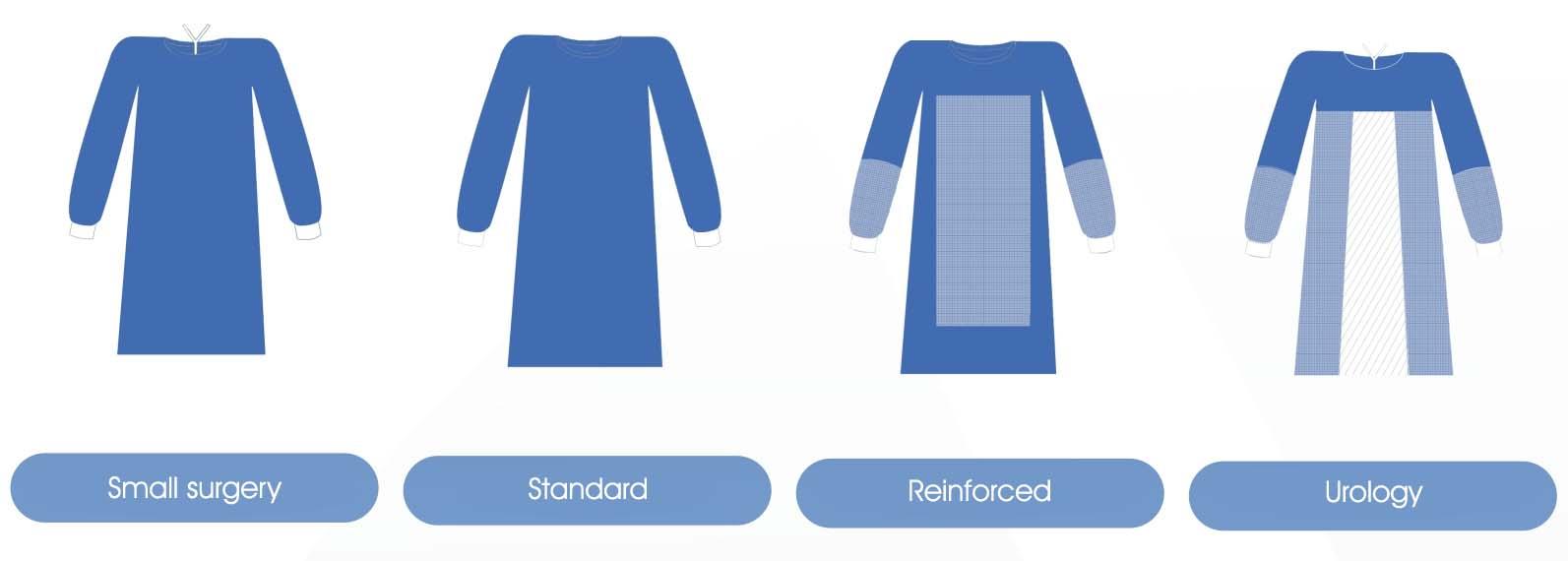
The various types of surgical gowns mainly refer to the AAMI levels of protection that the gown offers. However, manufacturers may choose to differentiate their surgical gowns by reinforcing various parts for specific procedures. For example, a urology surgical gown may have reinforced arms below the elbows along with reinforced material below the bust.
That said, the AAMI standards should still be the starting point for hospitals to select their product mix, as there are surgical gowns on the market that fail to provide adequate protection in crucial areas.
4. What’s the Difference Between an Isolation Gown and a Surgical Gown?
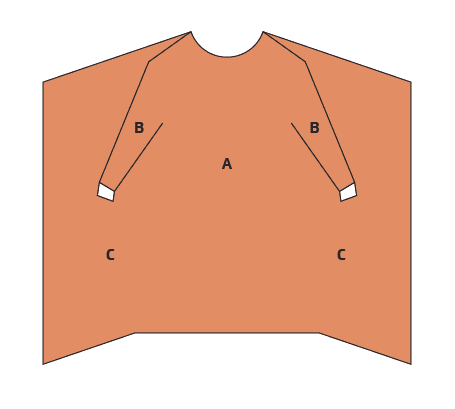
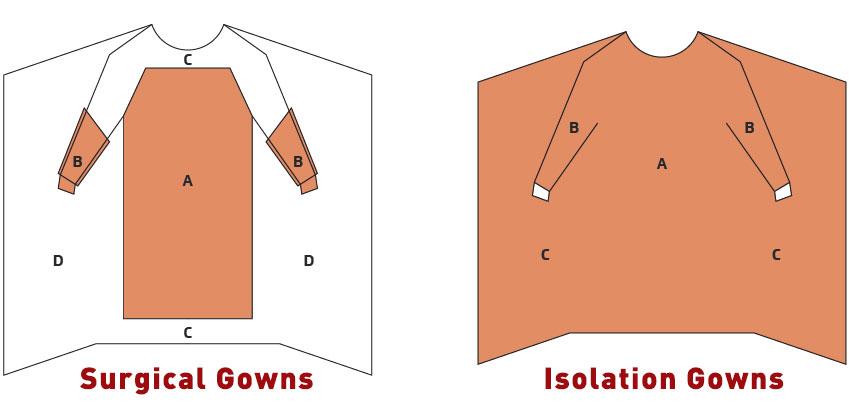
The main difference between surgical gowns vs isolation gowns is the designated critical zones of protection.
In surgical gowns, the critical zones include:
- the front of the body from the top of shoulders to knees
- the arms from the wrist cuff to above the elbow
Whereas in isolation gowns, the critical zones of protection are far larger and include almost the entire gown, minus the bindings, cuffs, and hems.
This picture depicts the difference in critical zones:
5. What Are Surgical Gowns Made of?
Traditionally, surgical gowns were tightly woven with cotton muslin and treated with fluid repellant. As technology advanced, manufacturers realised that muslin had low resistance to liquid penetration.
Now, most reusable gowns are manufactured with polyester or a polycotton blend and reinforced with coatings, laminates, or plastic film.
Tightly-woven polyester fabrics are usually stiffer and run hotter, making polyester gowns uncomfortable for healthcare workers. Polycotton blends are more comfortable but not as great as a liquid barrier.
Disposable surgical gowns are made of lightweight nonwoven fabrics such as spunlace, spunbond-meltblown-spunbond (SMS), and wet-laid. Of these three, one study found that nonwoven fabrics with SMS structure had the same level of comfort as microfiber garments.
6. Are Surgical Gowns Reusable?
Woven surgical gowns are reusable, but with a caveat: the protective properties of the gown tend to fade with repeated wetting or laundering. It’s for this reason that most surgeries these days are performed using disposable surgical gowns or drapes, despite the environmental impact and greater cost over time.
Textile technology and medical knowledge are constantly improving, however. It was only in 1952 that the surgical community realised that cotton muslin became an ineffective barrier once it was wet. But only in 1995 did we finally reach a consensus on standards to evaluate medical apparel.
Just recently, a study evaluating disposable versus reusable medical gowns found that Level 1 and 2 disposable gowns on the market did not meet AAMI specifications for impact penetration water resistance. That means that putting aside the greater costs and carbon footprint, disposable gowns also may not protect healthcare workers as well as reusable ones.
This, combined with the shortage of PPE, is partly why the Center for Disease Control (CDC) recommended a shift to “cloth gowns” in March 2020. When laundered according to CDC-recommended wash procedures, the reusable medical gowns retained their protective properties even after 75 washes.
7. What are the AAMI Levels of Protection?
Along with the American National Standards Institute (ANSI), the Association of Advancement of Medical Instrumentation (AAMI) came up with standards to classify the liquid barrier protection of protective gowns.
Level 4 surgical gowns offer the highest protection, whereas Level 1 offers the least.
The table below elaborates on the AAMI levels of protection:
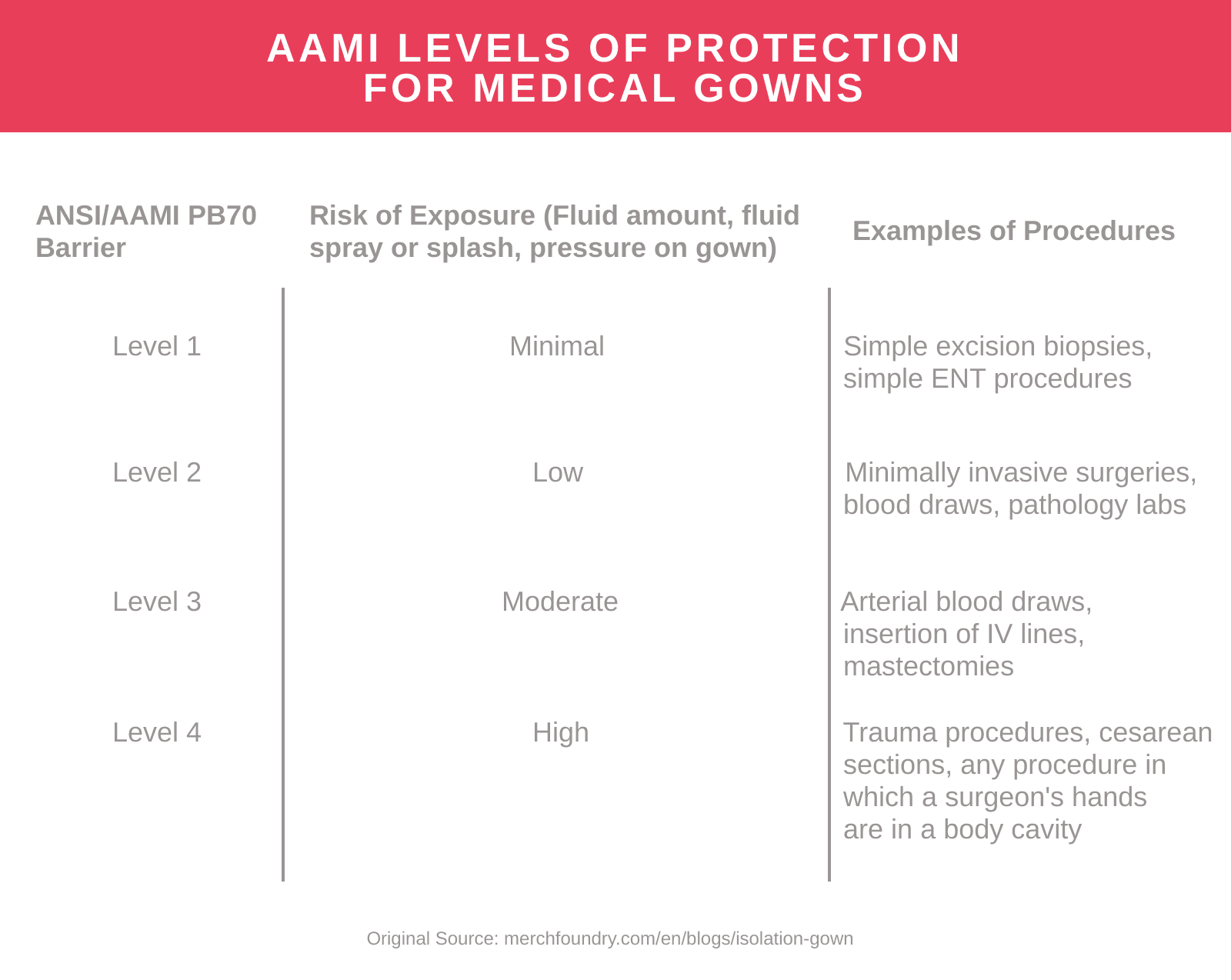
As long as they qualify under AAMI standards, these levels of protection are the same for both surgical and non-surgical gowns.
Product names on the market are non-standardised and can be confusing. Regardless of the product name, hospitals should look for product labelling that specifies the appropriate AAMI level of protection for procedures conducted in the healthcare facility.
8. What Should I Look For When Purchasing Surgical or Isolation Gowns?
Healthcare facilities purchase a mix of different gowns for patient-care procedures. When purchasing reusable or disposable surgical gowns, ask yourself five questions:
- What types of procedures are performed in the hospital/clinic?
- How many of these procedures do we perform in a given period, and how frequently?
- What’s the average time for each type of procedure?
- How much fluid will be present for each procedure?
- What’s the clinician’s role in each procedure?
Once answered, you can refer to the AAMI Levels of Protection as a starting point to determine the product mix along with the quantities necessary. Both under- and overprotection negatively impact healthcare outcomes.
That said, these other factors should also be considered:
- Ease of wear. In emergency situations, healthcare workers sometimes find that it takes too much time to don the proper equipment. This then leads to greater risks to the worker (if they choose not to wear the PPE) or to the patient (if it’s a matter of urgency).
- Comfort. Uncomfortable or poorly-designed PPE can contribute to lower performance or dexterity, especially during long procedures.
- Total cost. While disposable gowns may be the most convenient option, they may not be the most cost-effective — especially when coupled with the cost of proper waste disposal or incineration.
Manufacturing plants, hospitals & labs use MF to automate orders and manage their uniforms.
Learn more